Functions Of Skeletal System
Support
The skeleton provides the framework for the body. Bones provide the basic shape and structure for the body. What do you think we would look like if we didn't have bones? Pretty silly right? The bones are like the beams inside of a building, and all of our organs, muscles and skin are organized around the bones, just like the walls of a building. The mandible and maxilla support the tooth. Bones of the lower of the lower limbs, pelvis and vertebral column hold up the body.
Protection
The skeleton protects organs in the body. Bones can cover and protect many of out major organs. They are like an armor that protects our insides.
cranium: protects the brain
ribs/sternum: protects the lungs, heart and some digestive organs
pelvis: protects and supports the digestive and reproductive organs
spinal column: protects the spine
Blood Cell Production
Inside of the long bones in our bodies, there is a cavity that is filled with a substance called Bone Marrow. In this tissue, new blood cells are produced, and damaged blood cells are repaired. Red bone marrow produces red blood cells, white blood cells and other blood elements.
Movement
The bones are the levers that help the body move in different directions and in different ways. The bones by themselves can't move without the muscles that are connected to them.
Mineral Storage
Mineral is a substance that the body needs to carry out all of our bodily functions like thinking, breathing and moving around. One of the minerals that the body needs is calcium. Calcium is a major part of bone, and this is where the body stores its calcium. It is very important to make sure you eat enough calcium each day because if you don't get enough calcium, your body will take the calcium it needs from your bones. The less calcium the bone has, the weaker it will become.
BONE MATRIX
the collagen and mineral components
are responsible for major func.
charactristics of bone.
NOt enough mineral:causes bone to
be flexible and elastic
Not enough collagen:causes bone to
be brittle
Difference between cancellous and compact bone
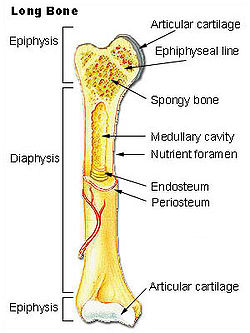
Compact bone
Compact bone or cortical bone is the outer shaft
of the bone. This is where the tissues are closely packed together giving a smooth and white
appearance to the bone. This part takes up nearly
¾ of the bone. There are cavities inside compact bones where bone marrow is stored. Compact bone
is thus primarily the outer surface of the bone.
It is also the shafts in long bones. It is
extremely hard bone with very few gaps inside and
the connective tissues being densely packed.
Cancellous bone
Cancellous or spongy bone tissues make up for most of the matter inside a bone. Here,tissues
are less densely packed giving it the appearance of a sponge (thus the name) Though it is softer than compact bone, it is really not spongy as the name suggests. It protects
internal organs and this is where blood is produced inside the body. It is also a store
house for minerals. Red and white blood cells
are manufactured here.
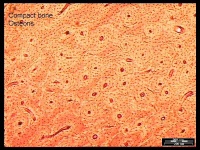
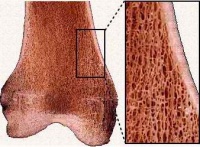
Compact bone (above) cancellous Bone (below)
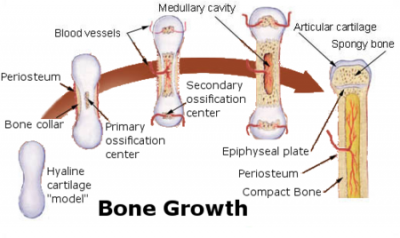
Endochondral ossification
Endochondral ossification
Endochondral ossification, on the other hand,
occurs in long bones and most of the rest of
the bones in the body; it involves an initial
hyaline cartilage that continues to grow.
The steps in endochondral ossification are:
Development of cartilage model
Growth of cartilage model
Development of the primary ossification center
Development of the secondary ossification center
Formation of articular cartilage and epiphyseal plate
Endochondral ossification begins with points in the cartilage called "primary ossification centers." They mostly appear during fetal development, though a few short bones begin their primary ossification after birth. They are responsible for the formation of the diaphyses of long bones, short bones and certain parts of irregular bones. Secondary ossification occurs after birth, and forms the epiphyses of long bones and the extremities of irregular and flat bones. The diaphysis and both epiphyses of a long bone are separated by a growing zone of cartilage (the epiphyseal plate). When the child reaches skeletal maturity (18 to 25 years of age), all of the cartilage is replaced by bone, fusing the diaphysis and both epiphyses together (epiphyseal closure).
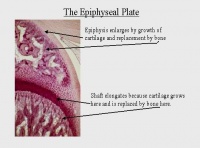
Epiphyseal Plate To Epiphyseal Line
The epiphyseal plate (or epiphysial plate,
physis, or growth plate) is a hyaline cartilage
plate in the metaphysis at each end of a long
bone. The plate is found in children and
adolescents; in adults, who have stopped growing,
the plate is replaced by an epiphyseal line.
Bone Repair
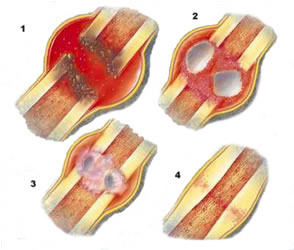
Reactive
After fracture, the first change seen by light and electron microscopy is the presence of blood cells within the tissues adjacent to the injury site. Soon after fracture, the blood vessels constrict, stopping any further bleeding. Within a few hours after fracture, the extravascular blood cells form a blood clot, known as a hematoma. All of the cells within the blood clot degenerate and die. Some of the cells outside of the blood clot, but adjacent to the injury site, also degenerate and die. Within this same area, the fibroblasts survive and replicate. They form a loose aggregate of cells, interspersed with small blood vessels, known as granulation tissue.
Reparative
Days after fracture, the cells of the periosteum replicate and transform. The periosteal cells proximal to the fracture gap develop into chondroblasts which form hyaline cartilage. The periosteal cells distal to the fracture gap develop into osteoblasts which form woven bone. The fibroblasts within the granulation tissue develop into chondroblasts which also form hyaline cartilage. These two new tissues grow in size until they unite with their counterparts from other parts of the fracture. These processes culminate in a new mass of heterogenous tissue which is known as the fracture callus. Eventually, the fracture gap is bridged by the hyaline cartilage and woven bone, restoring some of its original strength.
The next phase is the replacement of the hyaline cartilage and woven bone with lamellar bone. The replacement process is known as endochondral ossification with respect to the hyaline cartilage and bony substitution with respect to the woven bone. Substitution of the woven bone with lamellar bone precedes the substitution of the hyaline cartilage with lamellar bone. The lamellar bone begins forming soon after the collagen matrix of either tissue becomes mineralized. At this point, the mineralized matrix is penetrated by channels, each containing a microvessel and numerous osteoblasts. The osteoblasts form new lamellar bone upon the recently exposed surface of the mineralized matrix. This new lamellar bone is in the form of trabecular bone. Eventually, all of the woven bone and cartilage of the original fracture callus is replaced by trabecular bone, restoring most of the bone's original strength.
Remodeling
The remodeling process substitutes the trabecular bone with compact bone. The trabecular bone is first resorbed by osteoclasts, creating a shallow resorption pit known as a "Howship's lacuna". Then osteoblasts deposit compact bone within the resorption pit. Eventually, the fracture callus is remodelled into a new shape which closely duplicates the bone's original shape and strength. The remodeling phase takes 3 to 5 years depending on factors such as age or general condition.
CLICK HERE FOR ANATOMY OF SKELETAL SYSTEM
<<RETURN TO TOPICS>>